Diagnosis
Facial pigmentation and pigmented lesions are a common manifestation of photoaging and a frequent concern for patients presenting to aesthetic clinics.
The first step when assessing patients is to establish a diagnosis. This is usually a simple exercise.
However, when the diagnosis is not straightforward, I problem solve by going back to basic pathology and the different categories of disease:
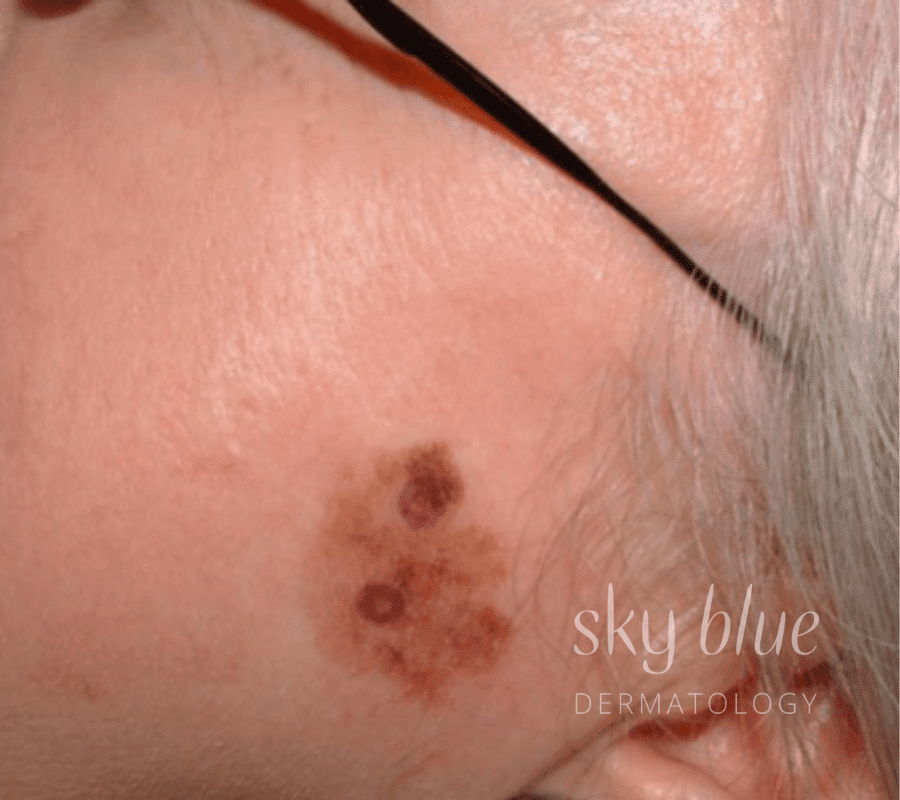
The most common pigmented lesions in photoaged patients are lentigines, seborrhoeic keratoses & pigmented solar keratoses. Be aware of less common lesions, particularly melanoma. Lentigo maligna is a subtype of melanoma that is easily missed and, therefore, something to keep in mind. Biopsy or referral to a dermatologist (or, if available, confocal microscopy) is much preferable to treating a lesion when the diagnosis is uncertain and essential when the possibility of melanoma exists.
Actinic dyschromia is a term that I use for diffuse or patchy and mottled pigmentation in patients with photoaging. Melasma can be similar in appearance, but the pigmentation that characterises melasma is usually more homogenous or even in colour, with a well-defined, irregular outline.
Treatment
Treatment will depend on the diagnosis, skin colour, budget and lifestyle issues.
Topical therapies include pigmentation blockers (e.g., hydroquinone), retinoids, vitamin C, niacinamide, and alpha hydroxy acids. For mild to moderate pigmentation, topical therapies are often combined with light chemical peels. Medium-depth peels are an option if more immediate results are desired and for more severe pigmentation.
In patients with advanced photoaging and pigmentation issues, medium-depth chemical peels can be used with cryotherapy to achieve excellent results. Keratotic lesions (e.g. macular seborrheic keratoses) are barriers to peeling solutions but will respond to liquid nitrogen cryotherapy. Caution – if performing peels and cryotherapy simultaneously, always peel before cryotherapy, as acid solutions penetrate more readily through areas treated by cryotherapy resulting in a deeper injury, with the potential to cause hypopigmentation and scarring.
Many laser and IPL devices effectively target pigmentation. As with other modes of treatment, achieving great results requires appropriate training and years of experience. The cosmetic nurses at Sky Blue have this training and experience and are experts in treating pigmentation with lasers and IPL.
Patients with skin types V and VI (dark brown to black) are more prone to post-inflammatory hyperpigmentation (PIH) and hypopigmentation with chemical peels, laser and IPL treatments. As with all patients, experience and caution are required when treating pigmentation, but this is even more important when managing individuals with darker skin types.
Our new UltraClear laser has become our favourite device for treating pigmentation. It allows greater levels of precision and the ability to treat other signs of aging with the “ultra” and “coring “modes.
In summary, pigmentation can be challenging, but the results achieved with the appropriate treatment modalities described above can be stunning and rewarding.
Diagnoses for title images
Image 1. This one is not easy. My diagnosis was Hori’s naevus (acquired bilateral naevus of Ota-like macules) and PIH due to a contact dermatitis caused by a whitening cream. Image 2. Melasma. Image 3. Solar lentigines. In photoaged skin, solar lentigines are often accompanied by epidermal thickening and can be difficult to differentiate from macular seborrheic keratoses. Image 4. Lentigo Maligna.









Sorry, the comment form is closed at this time.